Hone your POCUS interpretation and clinical reasoning by working through the interactive cases below.
Case #8: Hypoxemia in an immunocompromised patient
The POCUS consult team was asked to perform an urgent ultrasound for hypoxemia in a 30-year old inpatient.
The patient had been admitted for several weeks under the Hematology service. She had a history of an aggressive hematologic malignancy previously treated with chemotherapy, and appeared to be now having a recurrence of her cancer. Her recent stay had been complicated by multiple infections; including gram-negative bacteremia and persistent Candida fungemia (despite over a week of anti-fungal therapy).
Over the last 36 hours, she was noted to be increasingly tachycardic with soft blood pressures, for which she had received numerous fluid boluses. Her oxygenation had also deteriorated, and she was now requiring an FiO2 of 80% via HFNC to maintain saturations (previously on room air).
Other than her hematologic malignancy and recent complications, she had no significant medical history, and no known cardiopulmonary disease. An echocardiogram from 1 year prior was essentially normal.
The POCUS team was asked to specifically to assess her lungs to help determine the cause of her dramatically increased oxygen requirements.
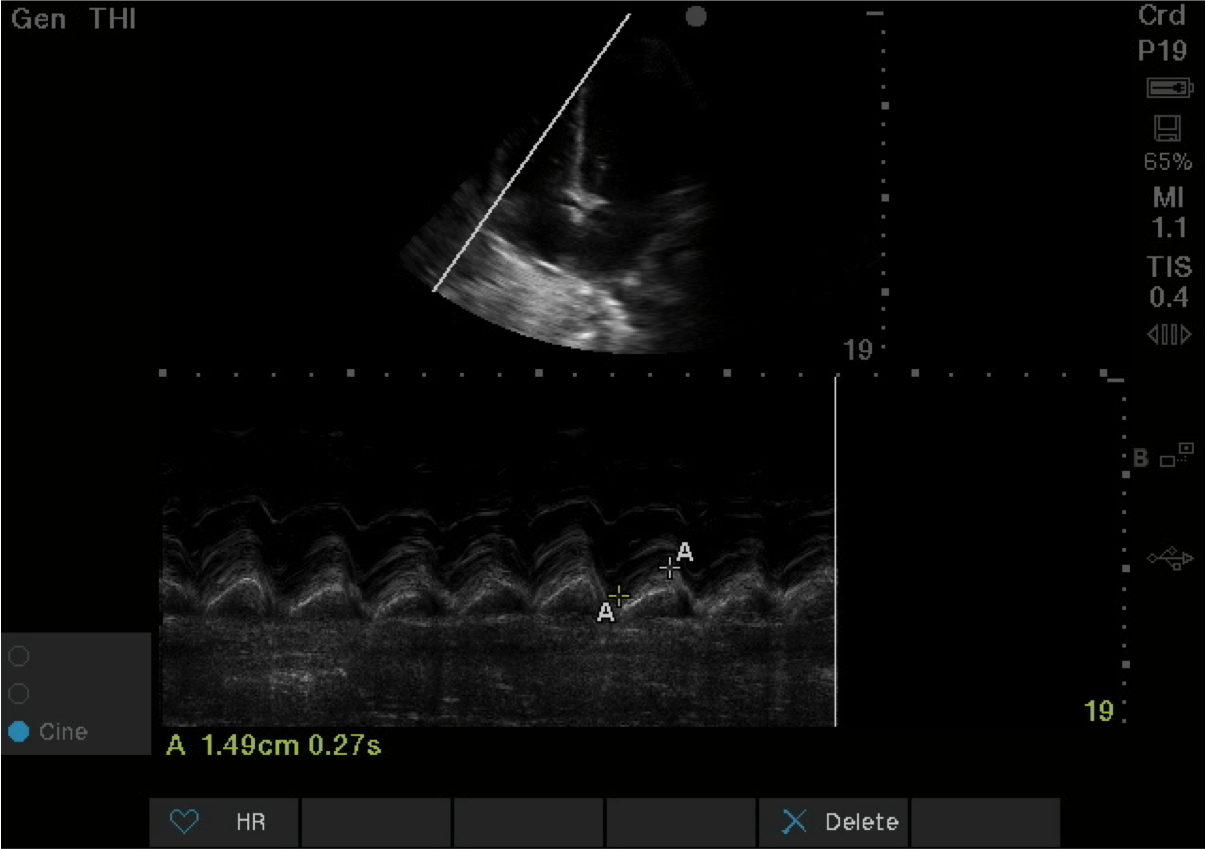
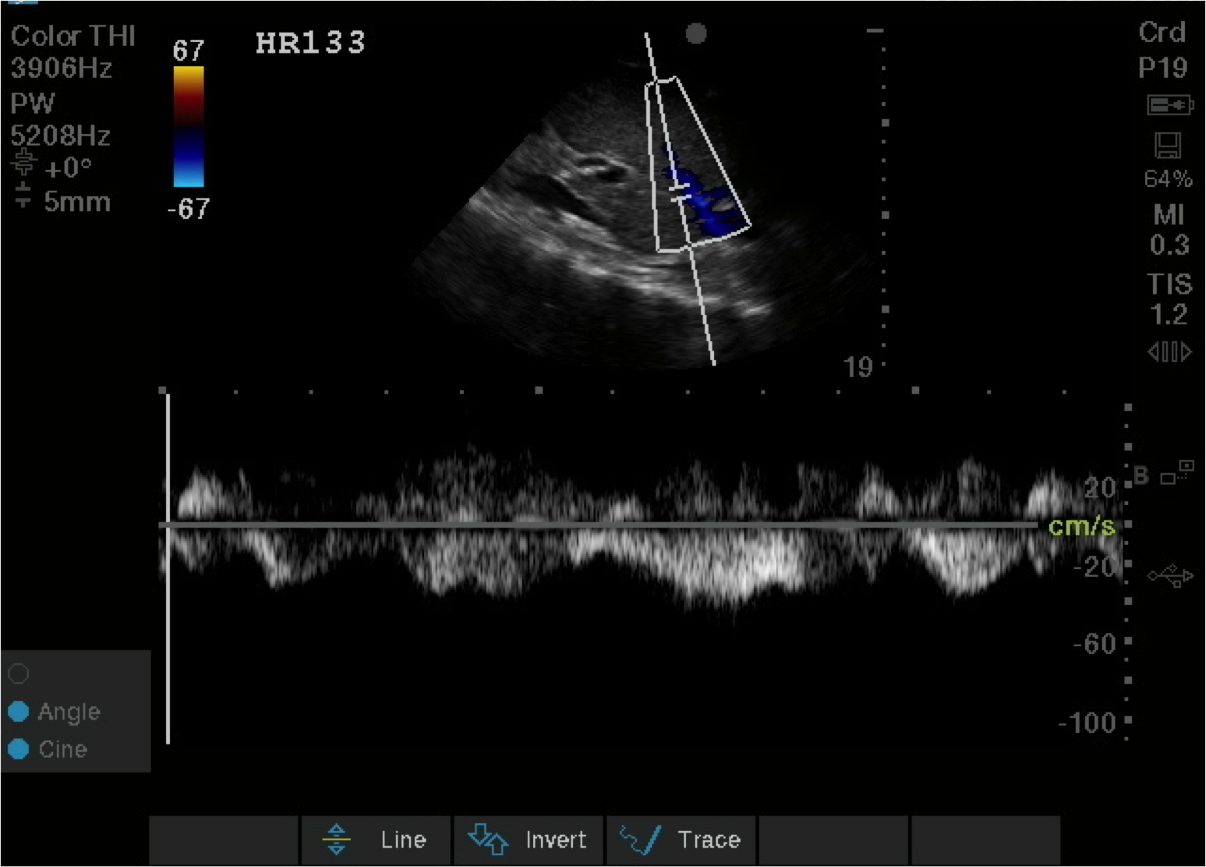
Before giving their clinical interpretation of the LUS findings, the POCUS team also scanned the heart and vasculature to obtain a more complete picture.
The patient was initiated on broad-spectrum antimicrobial therapy. Low-dose epinephrine was started to support her blood pressure, and she was intubated for respiratory support as her oxygen requirements and work of breathing continued to increase.
A comprehensive echocardiogram confirmed the POCUS findings. Her depressed LVEF was thought to be due to either septic cardiomyopathy or chemotherapy toxicity.
She had a prolonged stay in the ICU for respiratory failure/ARDS/pneumonia, but eventually was extubated and transfered back to the ward.
PoCUS Pearls
1. When scanning the lungs, a comprehensive, bilateral lung scan is far superior to a single clip; as this will offer more information and permit an interpretation based on the overall pattern of findings. Had this patient only had the R1 area scanned, for example, we may have reached the erroneous conclusion that her hypoxemia was likely due to pulmonary edema.
2. When scanning critically ill patients, it is almost always indicated to scan the heart, lungs, and vasculature together (as opposed to scanning a single system). You never know what you might find!