Hone your POCUS interpretation and clinical reasoning by working through the interactive case below.
Case #12: You “aor”ta check the CT! A cautionary tale…
Objectives:
1. What are some considerations with respect to performing thoracentesis?
2. What are the criteria for thorough assessment of a pleural effusion pre-thoracentesis?
3. An approach to reasoning through abnormal findings
ID: 77 F with history of COPD and thoracic aortic aneurysm, was electively admitted to cardiac surgery following aortic arch replacement with aortic arch vessel debranching, elephant trunk and bioprosthetic aortic valve replacement.
HPI: Post-operatively, she was found to have bilateral pleural effusions (L > R) requiring 6L of supplemental oxygen. She was started on Lasix, and was gradually weaned off oxygen, but despite continued to experience desaturations with ambulation limiting her discharge.
RFR: PoCUS team was asked to assess for therapeutic left thoracentesis to expedite discharge home.
Labs: WBC 9.2, Hgb 110, Plt 550. INR 1.1, PTT 29. Sodium 140, potassium 3.6, chloride 103, bicarb 29, urea 5.4, creatinine 36.
Imaging:
CT Chest with Contrast (1 week prior): Interval surgical repair of the ascending thoracic aorta with elephant trunk, aortic arch debranching and AV replacement. Perigraft fluid is present containing locules of gas within limits of the post op period.
CXR (2 days prior): Increased left pleural effusion, underlying atelectasis and/or consolidation. Patchy densities seen at the lateral right lung base consistent with a segment of atelectasis. No pulmonary edema seen.
POCUS Assessment - L4
Something isn’t right…
Further interrogation of the area, fanning from anterior to posterior:
Labelled Image
L4 short-axis view
Labelled Image - Short Axis
Review of Recent Imaging
Reviewing the CT chest report: “there is a descending aortic aneurysm measuring 6.6x6 cm, mildly increased in size since previous, with mural thrombus measuring 3.8cm in depth”
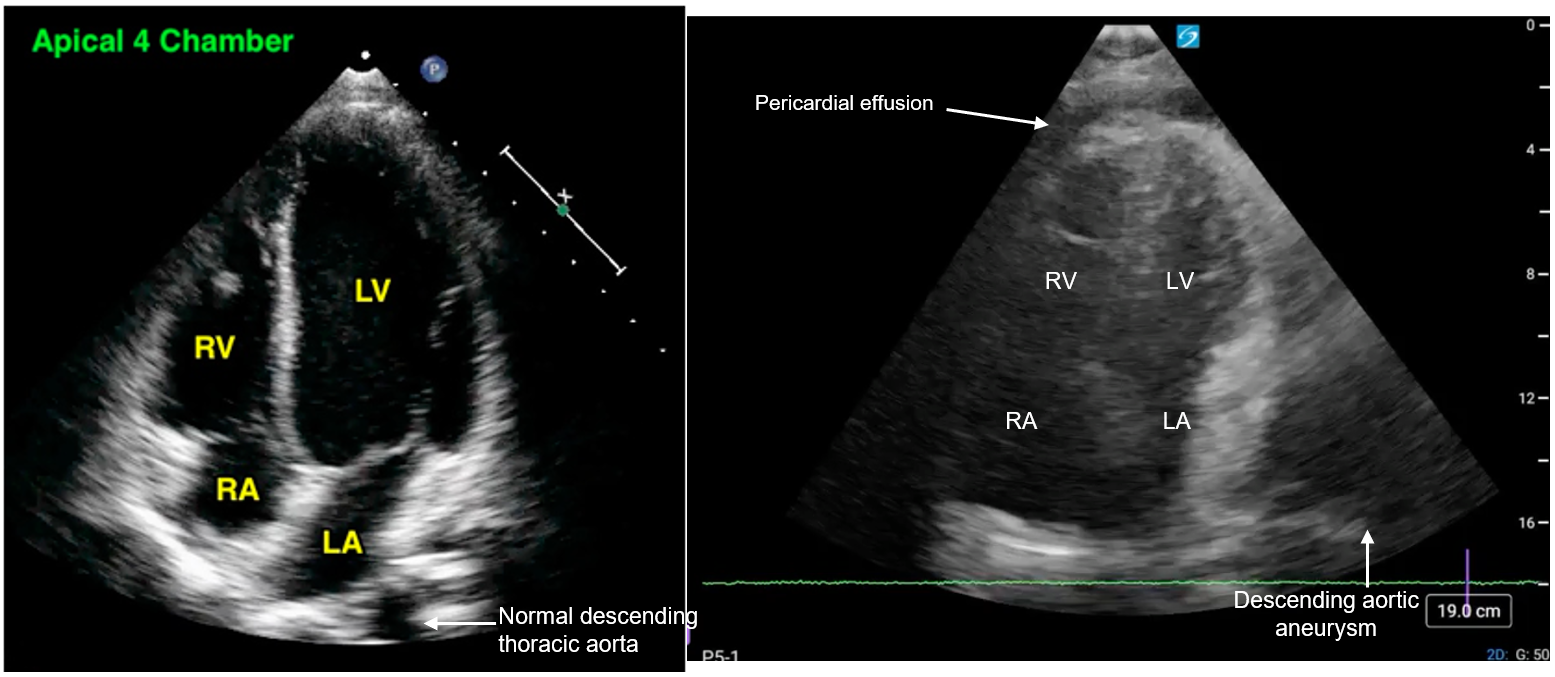
Cardiac POCUS
Labelled Image
Additional Consideration: Although not captured in this study, the colour doppler function could be used to assess for evidence of blood flow within a structure, if you are unsure whether it is a vessel.
Impression and Plan:
Pleural effusion was too small, aortic aneurysm was too big.
Patient was not very symptomatic, comfortable on room air.
The risks far outweigh the benefits of draining.
We recommended:
1)Trial of oral diuretics (lasix 40mg PO BID)
2)Continuing antibiotics for possible pneumonia
She was discharged and awaits outpatient TEVAR.