Hone your POCUS interpretation and clinical reasoning by working through the interactive cases below.
Case #3: Misadventures involving the right atrium
This was a 55-year old, otherwise healthy man presenting with a 3-week history of shortness of breath. He was treated as pneumonia as an outpatient without improvement, as subsequently presented to a peripheral hospital after having a positive D-dimer done at a walk-in clinic.
On assessment, he was hemodynamically stable with a BP of 134/78, HR of 88bmp, and sats of 93% on room air. Relevant lab work included a troponin-T of 33, and an NT-proBNP of 3005.
A CT PE protocol scan done by the ED team (prior to assessment by IM) revealed a saddle embolus, with filling defects seen in the R and L main PA, and extensive overall clot burden. Ultrasound of the legs also revealed a partially occlusive thrombus at the mid-thigh level of the superficial femoral vein.
Case Conclusion
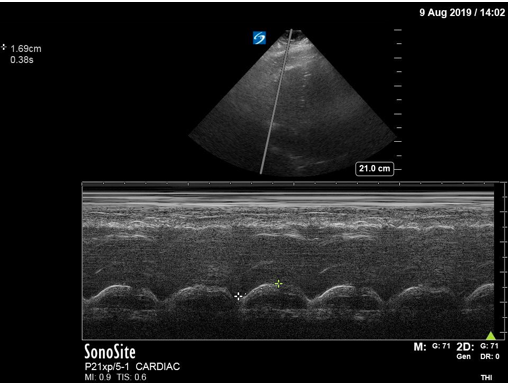
The patient had a Cardiology-performed echocardiogram, which confirmed the POCUS findings demonstrated above. It reported a markedly dilated RV, paradoxical septal motion consistent with elevated right-sided pressures, and an enlarged RA. There was confirmation of a clot-in-transit protruding from the RA into the RV. LV function was maintained, with an LVEF of 55%. Given the patient’s clinical stability, they were admitted to the Internal Medicine service and treated with IV heparin. They did well with this, and were eventually transitioned to a DOAC. No provoking factor was identified for the PE, and indefinite anticoagulation was recommended by Hematology given the severity of the presentation.
An important take-away from this case is the utility of POCUS for the diagnosis of PE (see the tables below). Certain signs, such as McConnell’s sign, paradoxical septal motion, or RV hypokinesis are quite specific for PE in the right clinical context - though their specificity decreases significantly in the presence of pre-existing cardiorespiratory disease. However, echo findings have poor sensitivity for PE - that is, a normal echo cannot rule out a PE. The exception to this is in hemodynamically unstable patients. If a PE is big enough to cause hemodynamic instability, the echo will be abnormal, with signs of RV dilation and RV strain. Thus, in a patient with shock NYD, a normal-appearing right ventricle is useful in ruling out PE as the cause of their hemodynamic instability.